Q&A: How you can counter coronavirus’ terrible toll on mental health
May is Mental Health Month! It may be eye-opening to learn that mental illnesses are common in the United States, with nearly one in five adults living with a mental health disorder, according to the National Institute of Mental Health.
Fewer than half ever get treatment. That’s a concerning trend during ordinary times. But these are extraordinary times, with New Jersey entering its third month of quarantine due to the coronavirus pandemic. Depression, fear, isolation, anxiety and more all have risen – and threaten to linger as the public health crisis evolves into an economic one.
We sat down with two mental health experts from Catholic Charities, Diocese of Trenton – Lisa Lawson, Director of Clinical and Integrated Health, and Danica Rivello, Director of Outpatient and Crisis Services (both pictured, right) – to learn about the link between the pandemic and mental health – and what people can do to protect themselves. (This conversation has been lightly edited for brevity and clarity.)
Q: What are the trends now in mental health?
Lisa: Mental health services have improved over the last 30 years, most notably with the Americans with Disabilities Act of 1990, and again when the law was revised in 2009. Following the ADA, we saw more evidence-based behavioral health treatments, increased federal funding, and a national recognition of the need to remove barriers to treatment. Fast forward a decade, and both the Protecting Access to Medicare Act and subsequent Excellence Act are responsible, in part, for enabling the creation and implementation of what we now call CCBHCs (Certified Community Behavioral Health Clinics, a model intended to increase community access to underserved people). Historically and even now, a large number of Americans with mental health disorders don’t get treatment. One recent trend that’s helped reverse that is the steady rise in web-based interventions, including Telehealth and Telemedicine. Brick and mortar locations can pose barriers for clients who lack transportation or are unavailable during their hours of operation. Telehealth, on the other hand, provides greater access to treatment, with additional benefits.
Loneliness, fear, stress
Q: This is a stressful time. How has the coronavirus crisis affected people’s mental health?
Danica: We are seeing more clients facing psychosocial stressors such as unemployment, lack of food, financial stressors, and isolation. If someone can’t meet their basic needs such as food, clothing and shelter, it’s harder for them to focus on their mental health needs and remain positive during these times. We are seeing clients experiencing increased loneliness due to stay-at-home and self-isolating orders. We also are seeing more anxiety, because people feel unsafe, worry about the present and the future, and fear the unknown.
 Lisa: There’s certainly been a disparate impact of COVID-19 on behavioral health. From increased isolation to firsthand association with those positive with the coronavirus, this is an understandably stressful time for most people. A pandemic like this affects people in a number of ways. Everyone handles stress, loss, and isolation differently – while some may enjoy the lack of social engagement, others struggle with increased depression and anxiety. There have been almost 100,000 coronavirus deaths in the U.S., and millions have been directly impacted by it. COVID-19 can heighten existing social inequities, especially in urban and rural areas. It is our responsibility, as social change agents, to recognize and address these inequities by expanding access to mental health resources for our most vulnerable populations.
Lisa: There’s certainly been a disparate impact of COVID-19 on behavioral health. From increased isolation to firsthand association with those positive with the coronavirus, this is an understandably stressful time for most people. A pandemic like this affects people in a number of ways. Everyone handles stress, loss, and isolation differently – while some may enjoy the lack of social engagement, others struggle with increased depression and anxiety. There have been almost 100,000 coronavirus deaths in the U.S., and millions have been directly impacted by it. COVID-19 can heighten existing social inequities, especially in urban and rural areas. It is our responsibility, as social change agents, to recognize and address these inequities by expanding access to mental health resources for our most vulnerable populations.
Operational changes
Q: As an essential provider, we have kept our mental health services open and operational through the pandemic. How has our staff changed what they do to ensure safety and comply with state mandates?
Lisa: We are functioning under heightened universal precautions while screening clients and staff in accordance with CDC guidelines. We have distributed personal protective equipment, including masks, gloves, and cleaning supplies, to staff and clients. Our facilities are regularly cleaned to ensure best health practices. And our medical staff screens clients and staff daily at our locations where in-person services continue. All programs are practicing social distancing for in-person, on-site interactions. Our Behavioral Health Services also offer Telehealth access, including video conferencing for individual and group therapy, as well as telephonic outreach for care coordination, case management, and wellness checks. Video translation services and bilingual staff also are provided on-site and telephonically as needed.
Danica: Our Guidance Clinic, Early Intervention Support Services, and Crisis Intervention Support Services programs are scrambling to re-conceptualize the delivery of services to ensure that we continue meeting the mental health needs of our clients during the pandemic. Clinicians have adjusted their clinical practices to provide services by telephone. Unfortunately, that means they miss out on building rapport face-to-face with clients and spotting cues and body language that can help them assess someone’s state of mind and needs. While most of our clients are opting to use telemental health services because they’re concerned about safety, we do continue to offer on-site services face-to-face. When we do see clients on-site, all staff adhere to the CDC guidelines by wearing face masks, maintaining 6 feet of social distance, and keeping a clean workplace.
Preparing for long-term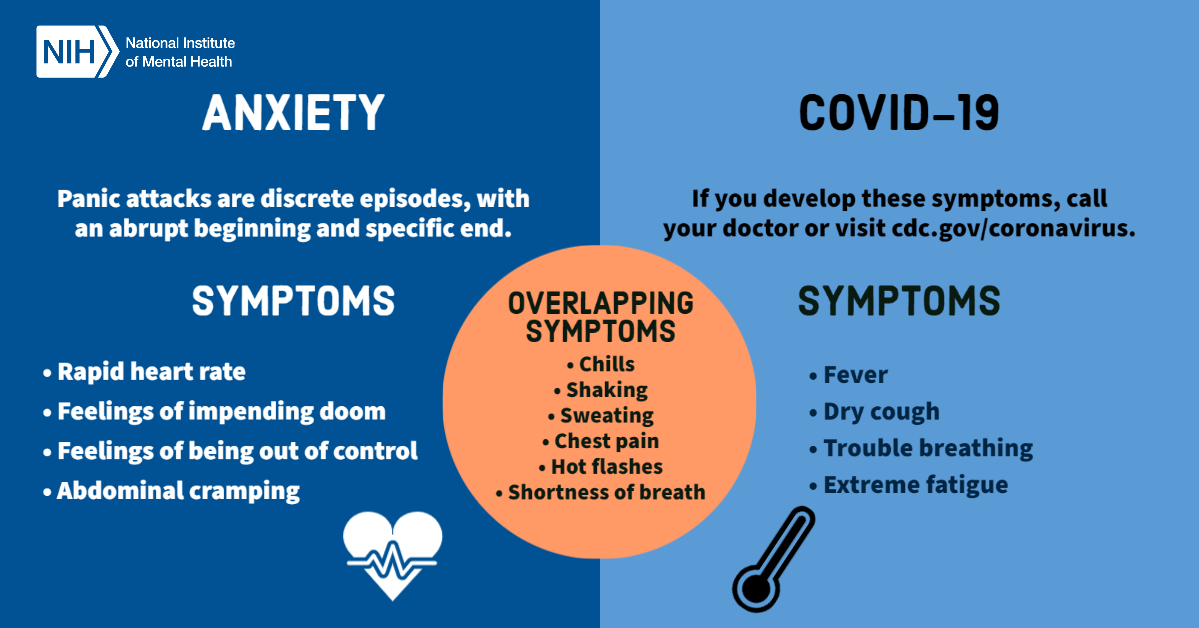
Q: The economic crisis caused by extended lockdowns is expected to impact folks’ mental health, long-term. How are you preparing for that?
Danica: Our care coordinators and case managers are familiarizing themselves with every and any resource available to people impacted by COVID-19. We’re also reaching out to clients to assess community needs, linking them to resources as appropriate, and helping them with obtaining federal stimulus checks and unemployment benefits, if eligible. Many clients who lost their jobs or had work hours cut during this crisis are newly eligible for services like food stamps and Medicaid, so we also are helping them connect with those services too.
Lisa: The coronavirus crisis is, essentially, a traumatic event that has caused mental trauma for many people. So we do expect to see long-term increases in anxiety and depression as a direct correlation to prolonged isolation, financial issues, and increased unemployment nationally, and of course, loss of life, employment, and social engagement. We also expect to see a rise in post-traumatic stress disorder, or PTSD. PTSD can occur following a single, or prolonged traumatic event. Symptoms include avoidance, increased reactivity, increased anxiety, and cognition and mood changes. PTSD should only be diagnosed by a clinically licensed professional, so anyone who believes they’re experiencing PTSD symptoms should follow up with a behavioral health professional.
Breaking the stigma
Q: A stigma persists. Any concerns this will keep folks from reaching out for help? How do you counter that?
Danica: Stigma can prevent people from seeking treatment and cause isolation and discrimination against people with mental illness. This stigma is especially dangerous because it is invisible. If someone breaks their leg and goes to the doctor, the fracture can easily be seen on an X-ray and there is no stigma with seeking out medical treatment. But in our society, too often the thinking is that someone should just pull themselves up by the bootstraps. This pandemic will hopefully reduce the stigma associated with mental health treatment, because everyone is being affected by the pandemic in one way or another and we are all truly in this together.
Lisa: Telehealth, unlike traditional methods of services, allows for greater anonymity. If someone is less inclined to seek services in-person, Telehealth offers a unique opportunity to reach out for help without the fear of stigma. Additionally, our agency employs a number of Peer Advocates and individuals with lived-experience in behavioral health to encourage treatment engagement.
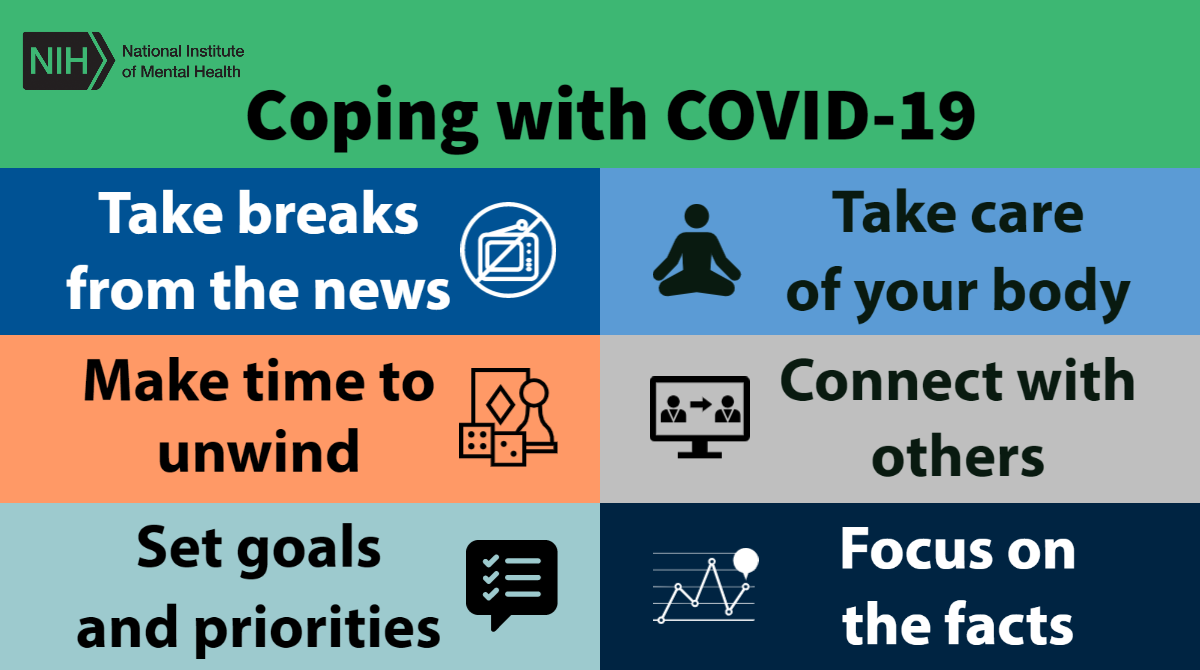
What you can do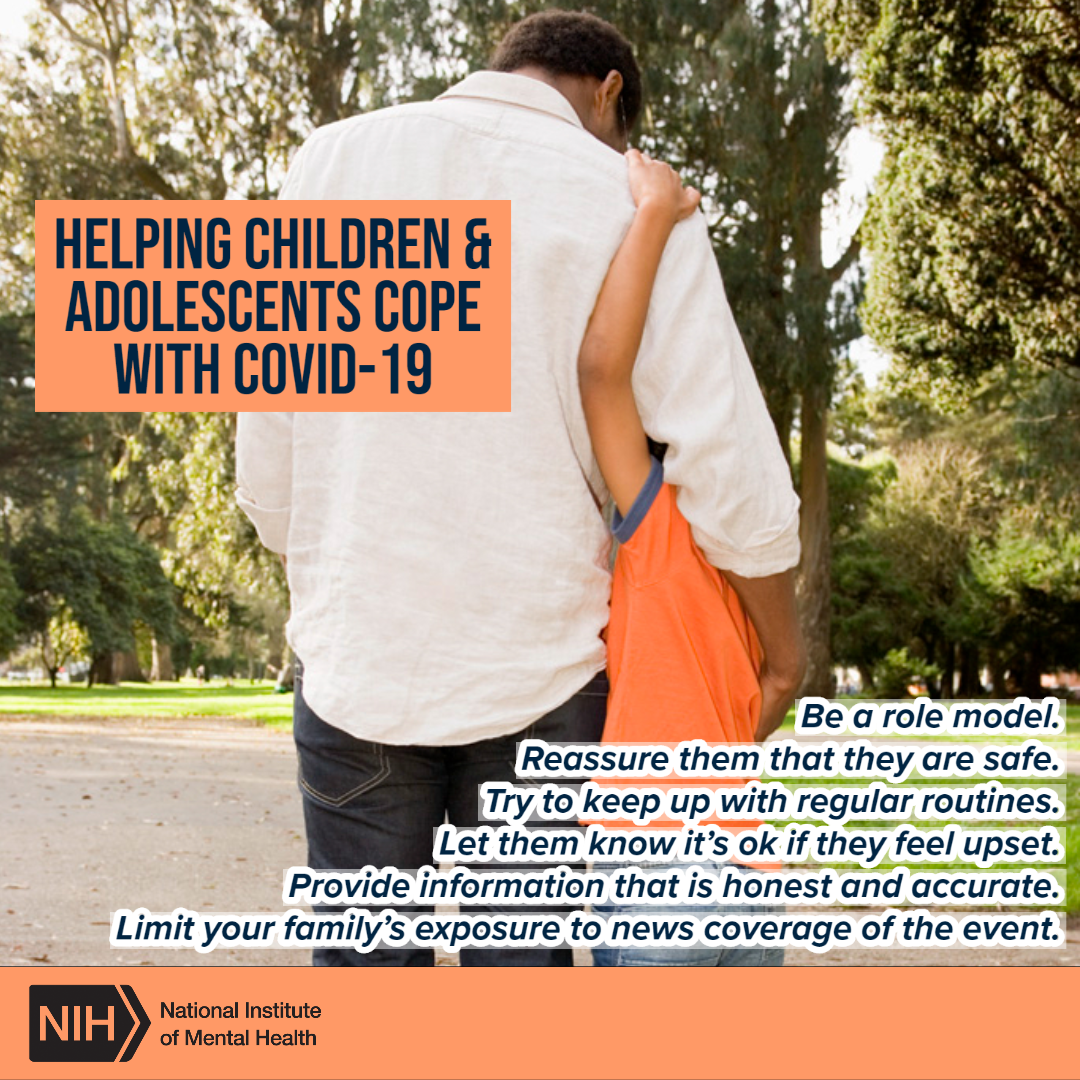
Q: What should people do if they need mental health help?
Lisa: Reaching out is a great first step towards recovery. Our Access, Help and Information Center (1-800-360-7711) is available to support anyone seeking services. Many of our facilities continue to offer walk-in admissions, as well as Telehealth for admission and subsequent appointments.
Danica: Mental health is just as important as physical health. People shouldn’t feel ashamed or embarrassed to reach out for help, because we all need help at various times in our lives. If someone has diabetes, they wouldn’t be ashamed to seek out treatment – they would see their doctor, discuss their symptoms, and develop a plan for a healthier lifestyle. When it comes to mental health treatment, a professional clinician will do the same thing – explore symptoms and teach coping skills to assist with life stressors, whether it be anxiety, depression or trauma.
Q: What should people do if they think their loved ones need help?
Lisa: Be present, however they can, for their loved one. The National Suicide Prevention Lifeline (1-800-273-8255) is a great tool for emergencies. Catholic Charities also offers emergency crisis support services to those in need of behavioral health treatment, seven days a week.
Danica: It can be heartbreaking to see a loved one struggling with mental illness. It may be hard to know how to best help and support your loved one. Every individual is different, and situations vary greatly. Try to show patience and caring, and avoid being judgmental. Listen to your loved one – don’t disregard or challenge the person’s feelings. Encourage them to talk with a mental health professional.
Q: Any encouraging words you might have for people struggling mentally during this crisis?
Lisa: I am often reminded of the Persian adage, “This too shall pass.” While the current state of this pandemic has increased feelings of isolation, fear, and hostility – in part due to misinformation and inequity – let’s use this opportunity to find a common ground where we can work together and share resources. This pandemic shall pass, so let’s come out of it stronger and more unified.
Danica: If you are struggling mentally during this worldwide crisis, please don’t be ashamed to reach out for help. We are here to help you!
About the experts
 Lisa Lawson is Catholic Charities’ Director of Clinical and Integrated Health. She is a licensed clinical social worker and MBA candidate. Lisa is a dynamic and team-oriented leader, with a proven record of generating and building relationships, managing programs, and implementing integrated healthcare practice in behavioral health settings. Lisa is driven by servant leadership, and is inspired to further organizational goals, while fostering professional development for those she serves. In her spare time, Lisa enjoys writing and contributing to topics related to social work development, philanthropy, and the application of industry best practice. Lisa also serves as a graduate field supervisor to emerging social work students, and is a proud member of the National Association of Social Work (NASW).
Lisa Lawson is Catholic Charities’ Director of Clinical and Integrated Health. She is a licensed clinical social worker and MBA candidate. Lisa is a dynamic and team-oriented leader, with a proven record of generating and building relationships, managing programs, and implementing integrated healthcare practice in behavioral health settings. Lisa is driven by servant leadership, and is inspired to further organizational goals, while fostering professional development for those she serves. In her spare time, Lisa enjoys writing and contributing to topics related to social work development, philanthropy, and the application of industry best practice. Lisa also serves as a graduate field supervisor to emerging social work students, and is a proud member of the National Association of Social Work (NASW).
 Danica Rivello is Catholic Charities’ Director of Outpatient and Crisis Services. She has worked in behavioral health for the past 20 years. Danica is a proud graduate of Widener University, where she obtained a Masters of Social Work. She is also a licensed clinical social worker and certified clinical supervisor and enjoys mentoring novice and seasoned therapists in the field. Danica provides administrative and clinical oversight to Early Intervention Support Services (EISS), Crisis Intervention Support Services (CISS), Guidance Clinic Outpatient Services, Capital Health Urban Care Coalition, and Prevention Plus. Danica is a member of the National Association of Social Workers (NASW) and unit chair for the NASW’s Gloucester/Camden/Salem chapter. For the past two years, Danica also has been Clinical Supervisor for a national agency that provides services to at-risk youth.
Danica Rivello is Catholic Charities’ Director of Outpatient and Crisis Services. She has worked in behavioral health for the past 20 years. Danica is a proud graduate of Widener University, where she obtained a Masters of Social Work. She is also a licensed clinical social worker and certified clinical supervisor and enjoys mentoring novice and seasoned therapists in the field. Danica provides administrative and clinical oversight to Early Intervention Support Services (EISS), Crisis Intervention Support Services (CISS), Guidance Clinic Outpatient Services, Capital Health Urban Care Coalition, and Prevention Plus. Danica is a member of the National Association of Social Workers (NASW) and unit chair for the NASW’s Gloucester/Camden/Salem chapter. For the past two years, Danica also has been Clinical Supervisor for a national agency that provides services to at-risk youth.
For help
To connect with professional, compassionate care, call our Access, Help and Information Center at (800) 360-7711.
Subscribe for more news
For more information, contact Lisa Lawson, director of Clinical & Integrated Health at Catholic Charities, at [email protected]; Danica Rivello, Director of Outpatient and Crisis Services, at (609) 256-4200 or [email protected]; or Dana DiFilippo, Catholic Charities communications, at [email protected] or (215) 756-6277 (cell).
To subscribe to our blog posts and news releases, fill out the fields below.

